How Compression Therapy Helps Heal Venous Leg Ulcers Effectively
Venous leg ulcers are a lot more common than most people realize, yet they often go overlooked until they become a debilitating issue. These stubborn wounds on the legs can disrupt daily life and take a significant toll on both physical and emotional well-being. The good news? They’re treatable, and one of the most effective methods is compression therapy.
This guide will walk you through what venous leg ulcers are, the role of compression therapy in their treatment, and how it can accelerate healing. Whether you’re dealing with a venous ulcer yourself or supporting a loved one, this post will provide vital, actionable insights.
Key Takeaways
- Venous leg ulcers result from poor circulation and can significantly disrupt daily life.
- Compression therapy effectively promotes healing by enhancing blood flow and reducing swelling.
- Professional healthcare guidance is crucial for both treating existing ulcers and preventing recurrence.
Introduction to Venous Leg Ulcers
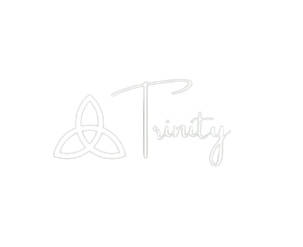
Venous leg ulcers, often referred to simply as leg ulcers, develop when veins in the legs fail to circulate blood effectively. Poor vein function leads to stagnant blood pooling and fluid buildup, which can cause open sores that are slow to heal.
These ulcers usually form above the ankles and are often accompanied by discomfort, swelling, and sometimes even severe infections. One treatment that consistently stands out for its proven effectiveness is compression therapy.
Compression therapy involves the use of specially designed stockings or bandages to apply pressure to the legs, promoting healthy blood flow and reducing swelling. This not only helps heal existing ulcers but also reduces the chances of new ones forming.
Causes of Venous Leg Ulcers
Understanding what causes venous leg ulcers is key to effective prevention and treatment. Here are some of the main contributors:
Poor Blood Circulation
Inefficient blood flow, often linked to conditions like varicose veins or chronic venous insufficiency, is one of the primary culprits.
Deep Vein Thrombosis (DVT)
Blood clots in the legs can impair circulation and lead to ulcers.
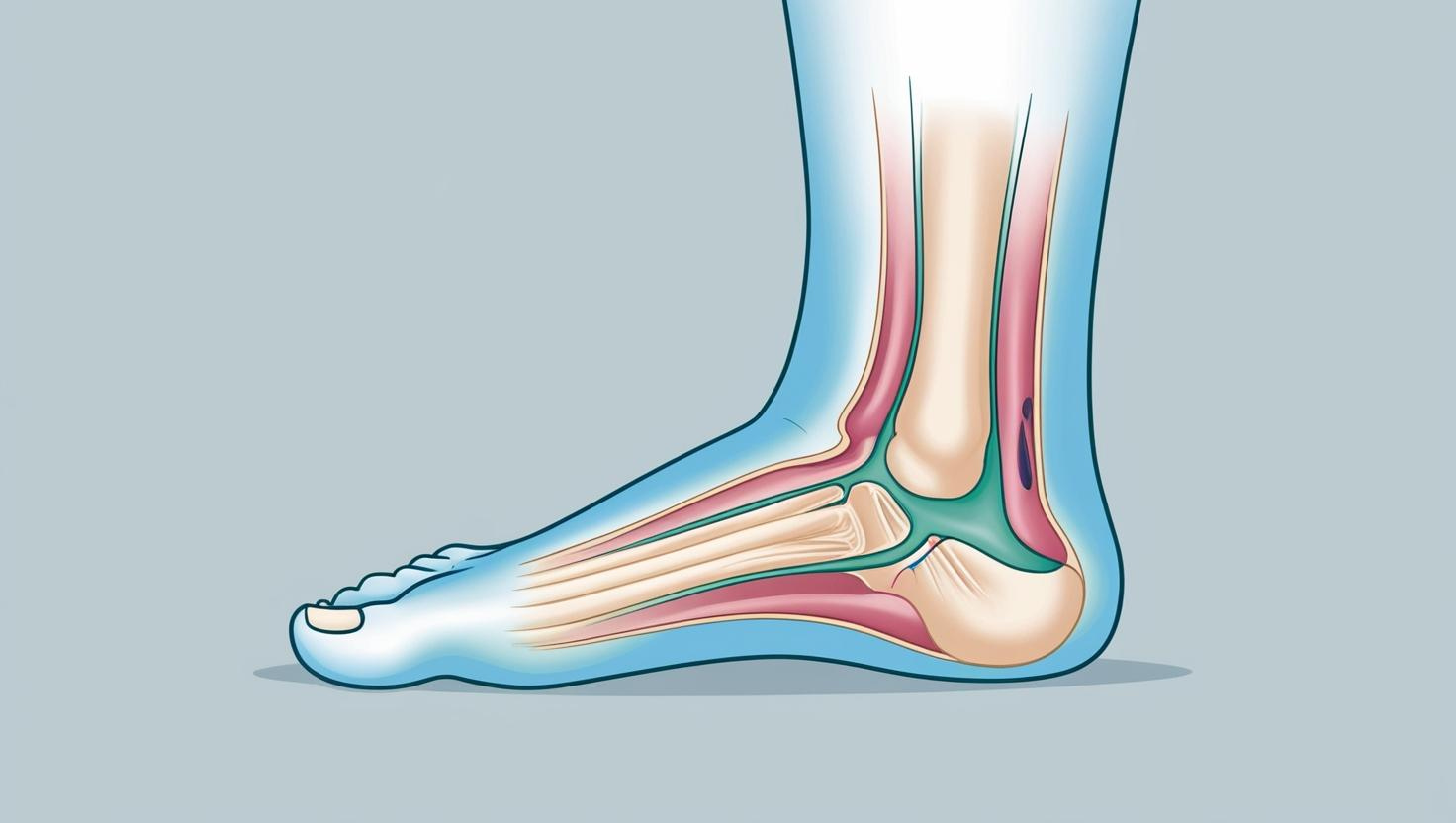
Lifestyle Factors
Obesity, a lack of physical activity, and unhealthy dietary habits can increase your risk.
Minor Injuries
Even small cuts or scrapes can escalate into ulcers if the veins fail to drain fluid effectively.
If you’ve noticed symptoms like swelling, discoloration, or chronic pain in the legs, consulting a healthcare professional is critical. Early diagnosis and intervention can dramatically improve outcomes, preventing more severe complications from developing.
Role of Compression Therapy

Compression therapy is widely considered the gold standard for treating venous leg ulcers. Here’s how it works and why it’s so effective:
Improves Vein Function
Applying pressure to the legs helps push blood back toward the heart, improving circulation.
Reduces Swelling
By minimizing fluid buildup, compression therapy alleviates one of the primary causes of discomfort.
Supports Healing
Increased blood flow delivers essential oxygen and nutrients to the affected area, which accelerates the healing process.
Customizable Application
From compression stockings to multilayer bandages, there are various wearable options tailored to different levels of vein dysfunction.
Regularly wearing compression stockings under the supervision of a healthcare provider can make a world of difference in both prevention and recovery. Additionally, a provider can recommend specific compression levels to match your individual needs, ensuring optimal effectiveness.
Preventing Blood Clots
Blood clots are a common, yet serious, complication linked to venous ulcers. But here’s the good news: compression therapy can help mitigate this risk.
How Compression Works
By improving blood flow and preventing fluid from pooling in the legs, compression therapy reduces the likelihood of clots forming.
Stay Consistent
It’s essential to wear compression stockings or bandages as prescribed to maintain steady circulation and prevent complications like deep vein thrombosis (DVT).
Preventing clots is more than just a precaution; it’s a crucial part of managing your overall vascular health. Incorporating regular physical activity and maintaining hydration can further enhance these preventative measures.
Deep Vein Thrombosis Considerations
Deep vein thrombosis (DVT) is a serious condition where blood clots form in the deep veins, often in the legs. Left untreated, these clots can lead to severe complications, including life-threatening pulmonary embolism.
Compression Therapy’s Role
By keeping blood moving efficiently, compression therapy minimizes the conditions that contribute to DVT.
Timely Intervention
If you experience symptoms like sudden swelling, pain, or redness in your legs, seek immediate medical attention. Time is critical when dealing with DVT.
With the guidance of a qualified healthcare provider, compression therapy can be a highly effective tool for both DVT prevention and treatment. Regular assessments and adjustments to your compression regimen ensure continuous protection against complications.
Treating an Infected Ulcer

Venous ulcers can sometimes become infected, which requires prompt and careful treatment. If left untreated, infections can lead to severe complications.
Antibiotics and Wound Care
Your healthcare provider may prescribe antibiotics to clear the infection, along with wound dressings to keep the ulcer clean and promote healing.
Compression Therapy
Ongoing compression treatment helps reduce swelling and supports faster recovery, even when the ulcer is infected.
Regular Cleaning
Keep the affected area clean and dry, and follow professional guidance on dressing changes.
Managing an infected ulcer successfully requires both effective medical interventions and commitment to proper wound care at home. Always adhere to your provider’s guidelines to prevent infection recurrence.
Managing Associated Symptoms

Beyond the ulcer itself, venous leg ulcers often bring other discomforts like pain, itching, and swelling. Fortunately, there are ways to manage these symptoms effectively.
Elevate the Leg
Keeping the affected leg elevated while resting can help reduce swelling and relieve discomfort.
Compression Therapy
Consistent use of compression stockings or bandages can alleviate many associated symptoms by improving circulation.
Skincare
Using moisturizers can minimize skin irritation, and anti-itch creams may help with itching.
Don’t hesitate to ask a healthcare provider about symptom management strategies tailored specifically for your condition. Incorporating a pain management plan or gentle exercises recommended by your healthcare provider can further improve comfort and quality of life.
The Role of a Healthcare Provider
When managing venous leg ulcers, expert guidance is essential. A healthcare provider offers more than just treatment recommendations; they partner with you for long-term health.
Tailored treatment plans, consistent monitoring, and proactive prevention strategies are just some of the benefits of working closely with your healthcare provider.
Take the First Step Toward Healing
If you or someone you know is struggling with a venous leg ulcer, expert help is just a call away. At Trinity Wound Care, our mobile healthcare clinic brings comprehensive, personalized wound care right to your doorstep in Las Vegas, NV.
Contact us today to learn how compression therapy can help you heal faster and reclaim your active lifestyle. Take control of your healing journey—schedule your consultation now.