Top Tips for Managing Pain During Wound Treatment Effectively
Wound treatment can often be a challenging experience, particularly when pain is involved. From minor injuries to chronic wounds like diabetic foot ulcers or pressure ulcers, managing pain during wound care is essential. Not only does effective pain management improve the healing process and overall quality of life, but it also reduces the risk of complications like infection.
Whether you’re a healthcare professional, caregiver, or patient, this guide offers a comprehensive breakdown of managing wound-related pain effectively. You’ll learn about pain types, strategies to assess and manage pain, and specialized care approaches for chronic wounds. Let’s get started!
Key Takeaways
Effective pain management not only accelerates wound healing but also significantly enhances patient comfort and quality of life.
Combining pharmacological and non-pharmacological strategies ensures a holistic approach to managing wound-related pain.
Chronic and neuropathic wounds require specialized care plans tailored to each patient’s specific needs.
Introduction to Wound Care
Wound care involves the management of wounds to promote healing while minimizing discomfort and preventing infection. From acute wounds like surgical cuts to chronic wounds like venous leg ulcers, each scenario requires a tailored care approach.
Why is effective wound care so important? For starters, untreated pain can slow recovery, lead to complications, and negatively impact mental well-being. Organizations such as the European Wound Management Association stress the importance of addressing not only wound care itself but also the pain that comes with it.
Understanding the various factors contributing to wound pain allows healthcare professionals to customize treatment plans that prioritize patient comfort.
Understanding Pain Types
To develop an effective pain management strategy, it’s important to understand the various types of pain experienced during wound care. Each type of pain requires a different clinical approach for optimal relief.
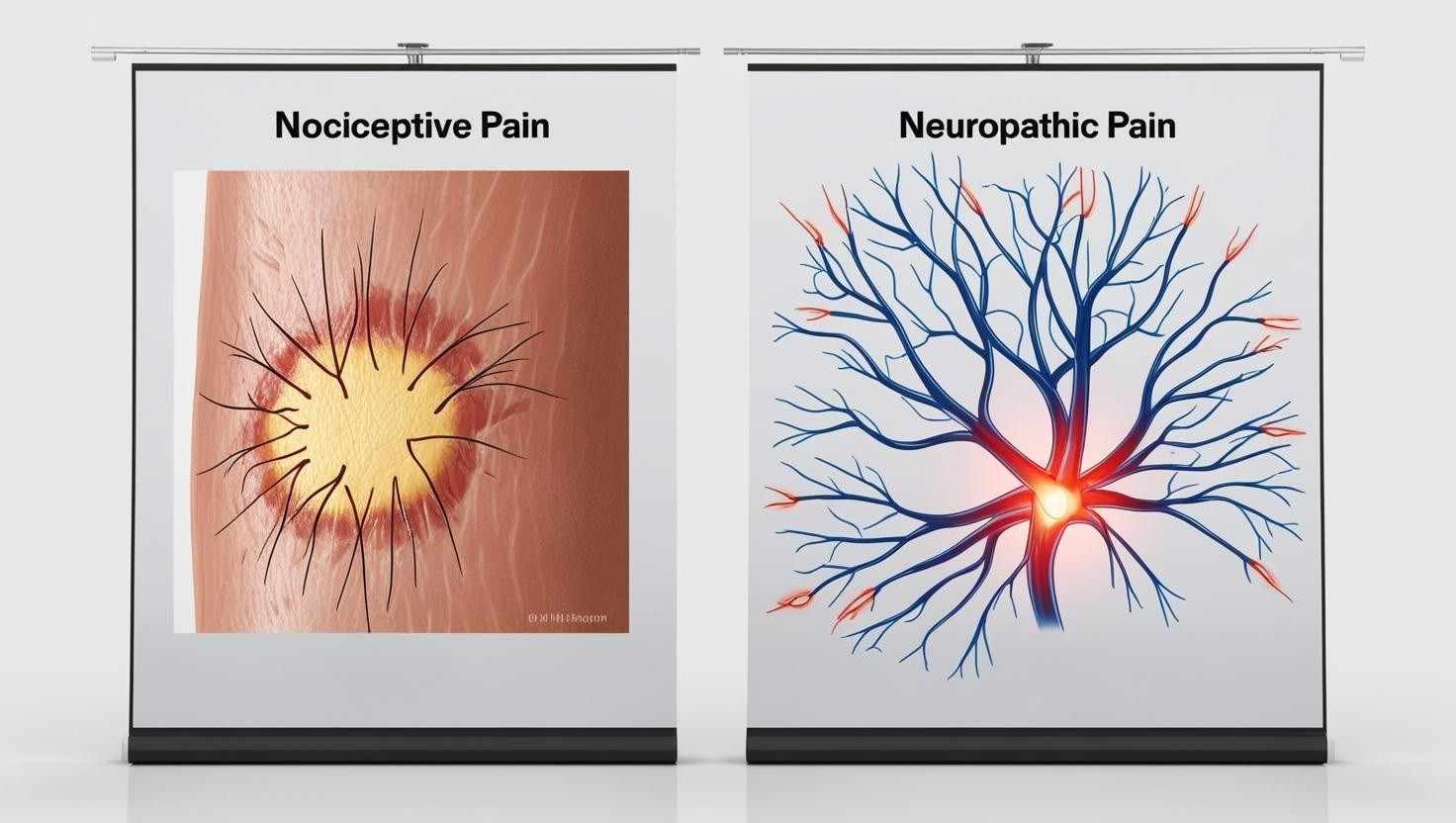
Nociceptive Pain
Nociceptive pain is caused by tissue damage and is usually localized, arising directly from the wound. This type of pain is often described as sharp, throbbing, or aching.
Neuropathic Pain
Neuropathic pain originates from nerve damage and can be more complex and widespread. Patients often describe it as burning, tingling, or shooting sensations.
Chronic Wound Pain
Chronic wound pain typically features a combination of nociceptive and neuropathic elements, making it particularly challenging to manage. A comprehensive, individualized approach is often necessary.
Understanding these distinctions allows healthcare providers to implement pain management techniques that are precise and effective.
Assessing Pain

Proper assessment is the cornerstone of any successful pain management plan. Consistently evaluating a patient’s pain experience helps tailor treatments and monitor progress over time.
Validated Pain Scales
Tools like numeric rating scales and visual analog scales are crucial for quantifying pain intensity. They provide a simple yet effective way for patients to communicate their pain levels.
WHO Guidelines
Following World Health Organization (WHO) protocols ensures a thorough understanding of pain, considering intensity, location, and duration. These details are essential in crafting a well-rounded care plan.
Types of Pain to Assess
Clinicians should differentiate between procedural pain (such as pain during dressing changes), background pain (constant pain), and breakthrough pain (sudden spikes). Addressing each type ensures comprehensive pain control.
Incorporating emotional and psychological factors into pain assessments can also provide deeper insight into the patient’s overall experience.
Pain Management Strategies

Effective pain relief during wound care requires a multifaceted approach. Both medications and non-pharmacological methods play key roles in alleviating discomfort.
Pharmacological Methods
Medications are often the first line of defense when addressing wound-related pain.
Topical Analgesics
Applied directly to the wound, topical analgesics provide localized relief with minimal systemic effects.
Systemic Painkillers
Drugs such as acetaminophen, NSAIDs, or stronger prescription medications help manage more severe or widespread pain.
Adjuvant Medications
For neuropathic pain, anticonvulsants and certain antidepressants may be prescribed to target nerve-related discomfort.
Non-Pharmacological Methods
Non-drug interventions can significantly enhance comfort, especially when combined with medications.
Transcutaneous Electrical Nerve Stimulation (TENS)
This technique uses low-level electrical currents to disrupt pain signals, offering additional relief.
Relaxation Techniques
Guided imagery, deep breathing, and mindfulness can help patients cope with and reduce their perception of pain.
Wound-Care Adjustments
Modifying care routines—such as minimizing dressing changes or ensuring wounds stay well-hydrated—can greatly reduce irritation and procedural pain.
Collaborative care involving nurses, physicians, and therapists is key to maximizing the benefits of these strategies.
Chronic Wounds

Chronic wounds, such as diabetic foot ulcers or venous leg ulcers, often require specialized interventions to manage both healing and pain effectively.
Negative Pressure Wound Therapy (NPWT)
NPWT uses suction to remove fluids and promote wound closure, often speeding up healing while also reducing discomfort.
Wound Cleansing and Debridement
Regular cleaning and removal of dead tissue are essential to prevent infection and manage pain associated with chronic wounds.
Personalized Care Plans
Tailoring treatment to the individual’s specific wound type and pain characteristics ensures optimal results. This may include dietary guidance, mobility support, and close follow-up care.
Holistic support—ranging from education to mental health resources—can further improve patient outcomes.
Neuropathic Pain
Neuropathic pain can be especially challenging to manage, requiring a deep understanding of its underlying mechanisms.
Common Treatment Approaches
Anticonvulsants and Antidepressants
These medications are often effective in addressing nerve-related pain, providing much-needed relief for patients with chronic wounds.
Nervous System Targeting
Because neuropathic pain often stems from nerve and spinal cord issues, treatment plans need to be precise and monitored regularly for effectiveness.
By combining medications with supportive therapies like nerve blocks or alternative medicine approaches, care providers can deliver a well-rounded pain management plan.
Nociceptive and Neuropathic Pain Differences
Understanding the differences between nociceptive and neuropathic pain helps ensure patients receive accurate and effective care.
Key Differences
Nociceptive Pain
Typically localized and arising from tissue injury, nociceptive pain is more predictable and easier to manage with standard treatments.
Neuropathic Pain
Often more widespread and complex, neuropathic pain results from nerve damage and requires targeted therapies that go beyond traditional wound care.
Both pain types may coexist, necessitating a layered and adaptive management approach.
Basal or Baseline Pain
Basal pain serves as the foundational level of discomfort that patients feel continuously, even when no external factors are present. Addressing this type of pain is crucial to creating a stable foundation for broader pain management efforts.
Managing Basal Pain
Pharmacological Interventions
Scheduled medications ensure consistent pain relief, helping to stabilize the patient’s overall comfort levels.
Non-Pharmacological Interventions
Simple measures like stable dressing techniques and compression therapy (when appropriate) help maintain comfort between dressing changes or procedures.
Continual monitoring ensures that any changes in basal pain are identified and addressed promptly.
Minimizing Pain

Minimizing pain during wound care requires diligence, expertise, and a compassionate approach. Both the clinical and emotional aspects of care are vital to achieving the best results.
Strategies for Minimizing Pain
Use of Topical Analgesics
Applying these before dressing changes can significantly reduce procedural pain, making the process smoother for patients.
Gentle Wound Cleansing
Being mindful of pressure and technique during cleansing prevents additional trauma and irritation.
Properly Fitted Dressings
Dressings that are secure but not too tight help maintain comfort and support the healing process.
A strong partnership between healthcare providers and patients helps ensure pain management remains effective and responsive to changing needs.
Take the Next Step in Pain Management
Pain should never stand in the way of recovery. Whether you’re managing a minor wound or dealing with the challenges of chronic wounds, effective pain management is critical to successful healing.
Trinity Wound Care offers expert, mobile wound care services across Las Vegas, delivering personalized care right to your doorstep. Don’t let wound pain control your life—reach out to Trinity Wound Care today to experience compassionate, comprehensive wound care tailored to your needs.